Webinars
Risks and Responsibilities
The reported benefits of home hemodialysis may not be experienced by all patients.
Despite the health benefits that home and more frequent hemodialysis may provide to those with chronic kidney disease, these forms of therapy are not for everyone. Please review this information carefully and discuss it with your doctor as you evaluate your therapy options.
Personal and Partner Responsibility
Home hemodialysis with the NxStage System during the day may not require a care partner, provided a physician and a qualified patient agree that solo home hemodialysis is appropriate. Patients performing nocturnal treatments are required to have a care partner. Care partners are trained on and follow guidelines for proper operation. If you choose to do more frequent home hemodialysis, you will be responsible for complying with your dialysis prescription, which may require treatments up to six days per week.
If you choose to do home hemodialysis alone during the day, you will need to take on the responsibility for tasks that would normally be taken care of by staff when in-center. You will need to perform all aspects of dialysis treatment from start to finish, including equipment setup, needle insertions, responding to and resolving system alarms, and system tear-down after treatment. In addition, you must monitor your blood pressure, ensure proper aseptic technique is followed, and follow all the training material and instructions given to you by your training nurses. You will also be trained on and need to know how to respond to health emergencies that might happen during treatment at home, including dizziness, nausea, low blood pressure, and fluid or blood leaks.
Treatment Environment
You must ensure that you have a clean and safe environment for your treatments. You also need to set aside space in your home for the needed supplies.
Risks Associated with All Forms of Hemodialysis
All forms of hemodialysis involve some risks. These may include high blood pressure, fluid overload, low blood pressure, heart-related issues, vascular access complications, cramps, backache, headache, dizziness, nausea, an "off" taste in the mouth, fatigue, fever, chills, joint pain, itching, seizures or sinusitis.
All hemodialysis therapies also involve the use of medical devices that introduce the potential for additional risks including air entering the bloodstream, damage of red blood cells, inflammatory reactions, blood chemistry imbalances, blood loss due to clotting of the blood tubing set or accidental blood line disconnection or other leak, allergic reactions, and excess warming or cooling of the dialysate. In addition, dialysis patients may have other underlying diseases that may, in some cases, make it more difficult for them to manage their hemodialysis treatments.
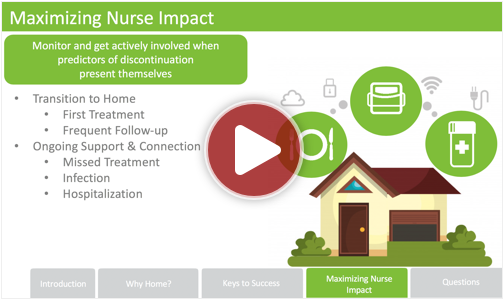
Risks associated with More Frequent Home Hemodialysis
Studies suggest that patients performing more frequent home hemodialysis may experience slightly fewer complications associated with their treatments and may experience improved clinical outcomes. However, there are certain risks unique to treatment in the home environment. Treatments at home are done without the presence of medical personnel and on-site technical support. Patients (and their care partners, if required), must both be trained on what to do and how to get medical or technical help if needed. When vascular access is exposed to more frequent use, infection of the site, and other access related complications may also be potential risks.
Risks Associated with Solo Home Hemodialysis Therapy
A qualified patient may dialyze alone, without a care partner present (solo home hemodialysis), provided the patient and physician agree that solo home hemodialysis is appropriate. Certain risks associated with hemodialysis treatment are increased when performing solo home hemodialysis because no one is present to help the patient respond to health emergencies. If patients experience needles coming out, blood loss, or very low blood pressure during solo home hemodialysis, they may lose consciousness or become physically unable to correct the health emergency. Losing consciousness or otherwise becoming impaired during any health emergency while alone could result in significant injury or death. Additional ancillary devices and training are required when performing solo home hemodialysis.
Increased Risks Associated with Home Nocturnal Hemodialysis Therapy
The NxStage System may be used at night while the patient and care partner are sleeping. Certain risks associated with hemodialysis treatment are increased when performing nocturnal therapy due to the length of treatment time and because therapy is performed while the patient and care partner are sleeping. These risks include, but are not limited to, blood access disconnects and blood loss during sleep, blood clotting due to slower blood flow or increased treatment time or both, and delayed response to alarms when waking from sleep. Treatment with nocturnal therapy may require adjustments to medications, including but not limited to iron, Erythropoiesis-Stimulating Agents (ESA), insulin/oral hypoglycemics, anticoagulants, and phosphate binders.
To view the on-demand archived presentations below you may need the WebEx player. Since the webinars are in different formats, please download the WebEx players for both .ARF and .WRF files.
Visit WebEx to download player (if required)
1. Gómez H, Kellum JA. Sepsis-induced acute kidney injury. Curr Opin Crit Care. 2016;22(6):546–553. doi:10.1097/MCC.0000000000000356
Professor of Medicine, Division of Nephrology, Barnes-Jewish Hospital; Washington University
St. Louis, MO
Professor of Medicine, Division of Nephrology, Barnes-Jewish Hospital; Washington University
St. Louis, MO
Membrana GmbH
Wuppertal, Germany
Membrana GmbH
Wuppertal, Germany
Chief, Renal Section, VA Pittsburgh Healthcare System.
Professor of Medicine, University of Pittsburgh School of Medicine. Pittsburgh, PA
The opinions expressed by Dr. Palevsky in this presentation are his own and do not represent the Department of Veterans Affairs. Nothing in his presentation should be construed to represent an endorsement of any specific products or services by the Department of Veterans Affairs.
Professor of Medicine, Director of the Division of Experimental Therapeutics,
Director of the Division of Nephrology, and Interim Chair of the Department of Medicine.
Columbia University, New York, NY
Professor and Vice-Chariman of Medicine for Clinical Affairs
Director, Division of Renal Diseases and Hypertension
University of Texas Medical School at Houston, Houston, TX
Nephrology Consultant – Burn Center
Doctors Hospital Burn Unit, Augusta, GA
Risks and Responsibilities
Renal replacement therapy, as with any medical therapy is not without risks. The decision of which therapy and medical device to use should be made by the physician, based on previous experience and on the individual facts and circumstances of the patient.
There is no literature demonstrating that one therapy is clinically better than the other.
The use of anticoagulation is at the discretion of the prescribing physician.